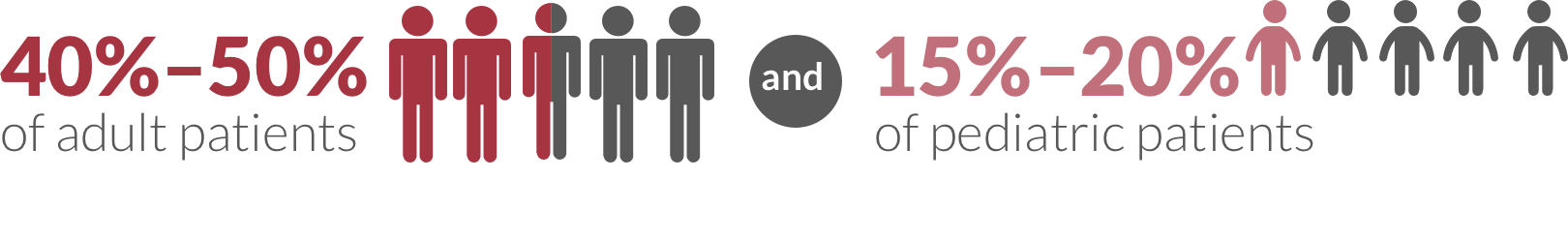
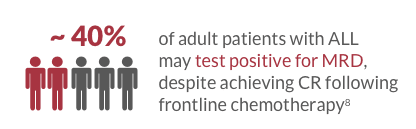
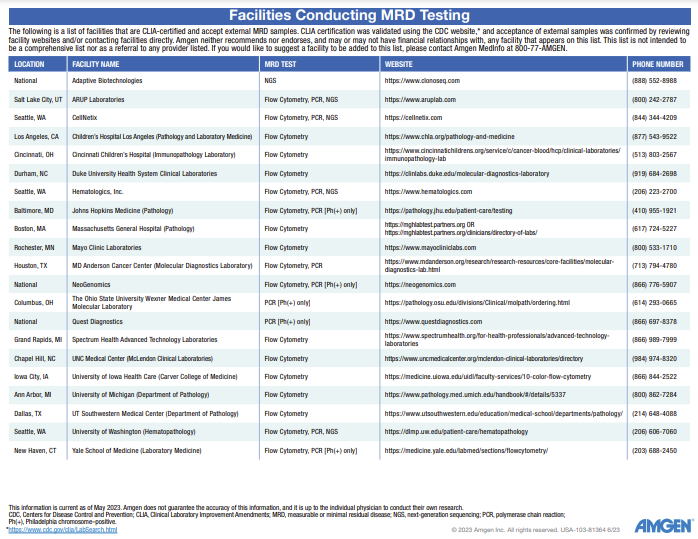
References: 1. National Cancer Institute. https://seer.cancer.gov/statfacts/html/alyl.html. Accessed June 08, 2023. 2. National Cancer Institute. https://seer.cancer.gov/statistics-network/explorer/application.html?site=92&data_type=4&graph_type=5&compareBy=age_range&chk_age_range_16=16&chk_age_range_62=62&chk_age_range_122=122&chk_age_range_160=160&chk_age_range_166=166&series=9&sex=1&race=1&hdn_stage=101&advopt_precision=1&advopt_show_ci=on&hdn_view=0&advopt_show_apc=on&advopt_display=2#resultsRegion0. Accessed June 05, 2023. 3. Hoelzer D. Monitoring and managing minimal residual disease in acute lymphoblastic leukemia. Am Soc Clin Oncol Educ Book. 2013;33:290-293. 4. Cooper SL, Brown PA. Treatment of pediatric acute lymphoblastic leukemia. Pediatr Clin North Am. 2015;62:61-73.
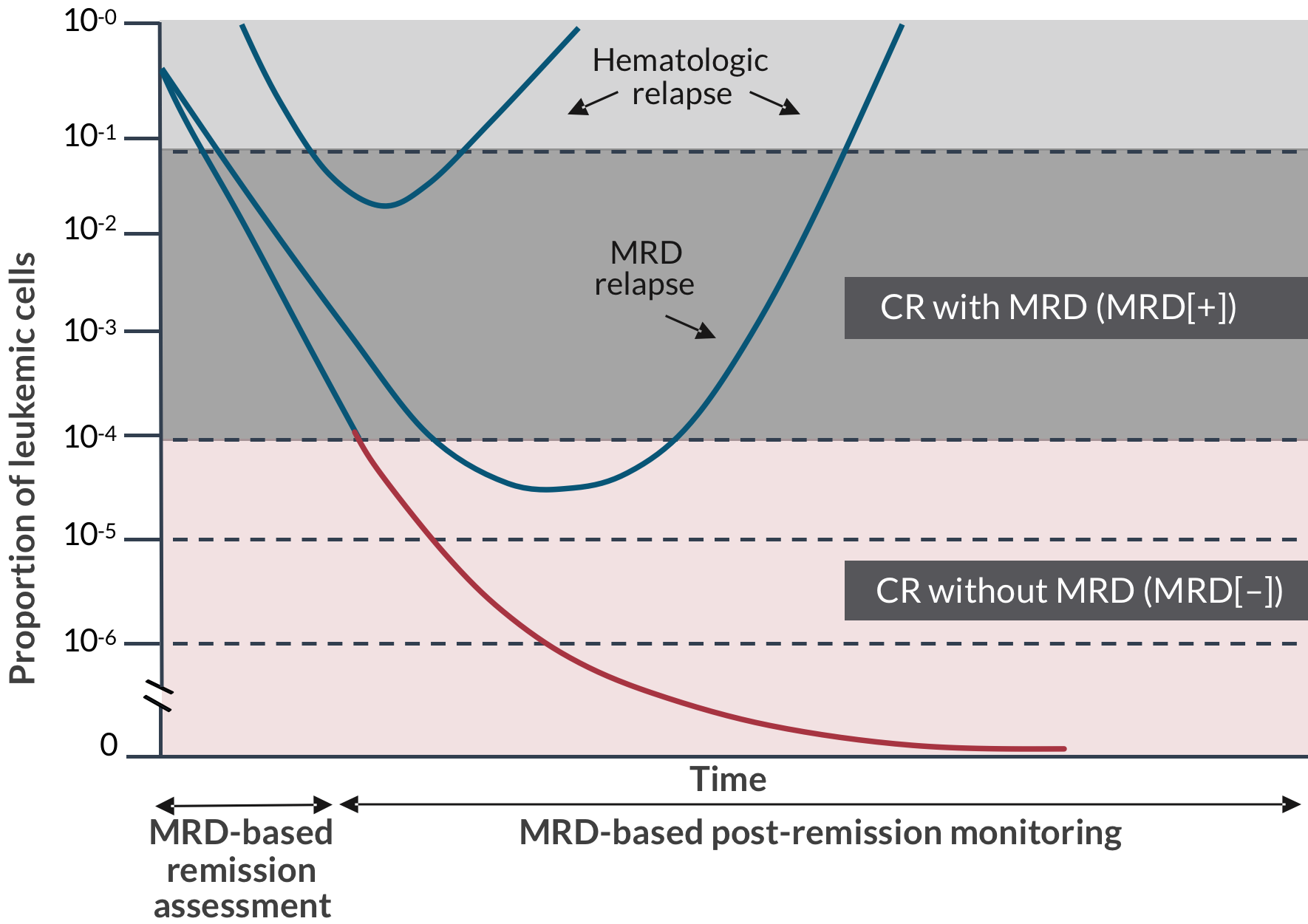
5. Campana D. Minimal residual disease in acute lymphoblastic leukemia. Semin Hematol. 2009;46:100-106. 6. Paganin M, Zecca M, Fabbri G, et al. Minimal residual disease is an important predictive factor of outcome in children with relapsed ‘high-risk’ acute lymphoblastic leukemia. Leukemia. 2008;22:2193-2200. 7. Akabane H, Logan AC. Clinical significance and management of MRD in adults with acute lymphoblastic leukemia. Clin Adv Hematol Oncol. 2020;18:413-422. 8. Brüggemann M, Raff T, Flohr T, et al. Clinical significance of minimal residual disease quantification in adult patients with standard-risk acute lymphoblastic leukemia. Blood. 2006;107:1116-1123. 9. Kotrova M, Trka J, Kneba M, et al. Is next-generation sequencing the way to go for residual disease monitoring in acute lymphoblastic leukemia? Mol Diagn Ther. 2017;21:481-492.
10. Chen X, Wood BL. How do we measure MRD in ALL and how should measurements affect decisions. Re: Treatment and prognosis? Best Pract Res Clin Haematol. 2017;30:237-248. 11. Short NJ, Jabbour E, Albitar M, et al. Recommendations for the assessment and management of measurable residual disease in adults with acute lymphoblastic leukemia: A consensus of North American experts. Am J Hematol. 2019;94:257-265. 12. Referenced with permission from the NCCN Clinical Practice Guidelines in Oncology (NCCN Guidelines®) for Acute Lymphoblastic Leukemia v.1.2023. ©National Comprehensive Cancer Network, Inc. 2023. All rights reserved. Accessed June 2, 2023. To view the most recent and complete version of the guideline, go online to NCCN.org. NCCN makes no warranties of any kind whatsoever regarding their content, use or application and disclaims any responsibility for their application or use in any way. 13. Referenced with permission from the NCCN Clinical Practice Guidelines in Oncology (NCCN Guidelines®) for Pediatric Acute Lymphoblastic Leukemia v.2.2023. ©National Comprehensive Cancer Network, Inc. 2023. All rights reserved. Accessed March 13, 2023. To view the most recent and complete version of the guideline, go online to NCCN.org. NCCN makes no warranties of any kind whatsoever regarding their content, use or application and disclaims any responsibility for their application or use in any way. 14. Helgestad J, Rosthøj S, Johansen P, et al. Bone marrow aspiration technique may have an impact on therapy stratification in children with acute lymphoblastic leukaemia. Pediatr Blood Cancer. 2011;57:224-226.