IMPORTANT SAFETY INFORMATION
WARNING: CYTOKINE RELEASE SYNDROME and NEUROLOGICAL TOXICITIES including
IMMUNE EFFECTOR CELL-ASSOCIATED NEUROTOXICITY SYNDROME
-
Cytokine Release Syndrome (CRS), which may be life-threatening or fatal,
occurred in patients receiving BLINCYTO®. Interrupt
or discontinue BLINCYTO® and treat with
corticosteroids as recommended.
-
Neurological toxicities, including immune effector cell-associated
neurotoxicity syndrome (ICANS), which may be severe, life-threatening or
fatal, occurred in patients receiving BLINCYTO®.
Interrupt or discontinue BLINCYTO® as
recommended.
Contraindications
BLINCYTO® is contraindicated in patients with a
known hypersensitivity to blinatumomab or to any component of the product
formulation.
Warnings and Precautions
- Cytokine Release Syndrome (CRS): CRS, which may be life-threatening or fatal, occurred in patients receiving
BLINCYTO®. The median time to onset of CRS is 2 days after the start of infusion and the median time to resolution
of CRS was 5 days among cases that resolved. Closely monitor and advise patients to contact their healthcare
professional for signs and symptoms of serious adverse events such as fever, headache, nausea, asthenia,
hypotension, increased alanine aminotransferase (ALT), increased aspartate aminotransferase (AST), increased total
bilirubin, and disseminated intravascular coagulation (DIC). The manifestations of CRS after treatment with
BLINCYTO® overlap with those of infusion reactions, capillary leak syndrome (CLS), and hemophagocytic
histiocytosis/macrophage activation syndrome (MAS). Using all of these terms to define CRS in clinical trials of
BLINCYTO®, CRS was reported in 15% of patients with R/R ALL, in 7% of patients with MRD-positive ALL, and in 16% of
patients receiving BLINCYTO® cycles in the consolidation phase of therapy. If severe CRS occurs, interrupt BLINCYTO®
until CRS resolves. Discontinue BLINCYTO® permanently if life-threatening CRS occurs. Administer corticosteroids for
severe or life-threatening CRS.
- Neurological Toxicities, including Immune Effector Cell-Associated Neurotoxicity Syndrome:
BLINCYTO® can cause serious
or life-threatening neurologic toxicity, including ICANS. The incidence of neurologic toxicities in clinical trials was
approximately 65%. The median time to the first event was within the first 2 weeks of BLINCYTO® treatment. The most
common (≥ 10%) manifestations of neurological toxicity were headache and tremor. Grade 3 or higher neurological toxicities occurred in approximately 13% of patients, including encephalopathy, convulsions, speech disorders, disturbances in consciousness, confusion and disorientation, and coordination and balance disorders. Manifestations of neurological toxicity included cranial nerve disorders. The majority of neurologic toxicities resolved following interruption of BLINCYTO®, but some resulted in treatment discontinuation.
The incidence of signs and symptoms consistent with ICANS in clinical trials was 7.5%. The onset of ICANS can be
concurrent with CRS, following resolution of CRS, or in the absence of CRS. There is limited experience with BLINCYTO®
in patients with active ALL in the central nervous system (CNS) or a history of neurologic events. Patients with a
history or presence of clinically relevant CNS pathology were excluded from clinical studies. Patients with Down Syndrome may have a higher risk of seizures with BLINCYTO® therapy; consider seizure prophylaxis prior to initiation of BLINCYTO® for these patients.
Monitor patients for signs and symptoms of neurological toxicities, including ICANS, and interrupt or discontinue
BLINCYTO® and/or treat with corticosteroids as outlined in the PI. Advise outpatients to contact their healthcare professional if they develop signs or
symptoms of neurological toxicities.
- Infections: Approximately 25% of patients receiving BLINCYTO® in clinical
trials experienced serious infections such
as sepsis, pneumonia, bacteremia, opportunistic infections, and catheter-site
infections, some of which were life-threatening or fatal. Administer
prophylactic antibiotics and employ surveillance testing as appropriate during
treatment. Monitor patients for signs or symptoms of infection and treat
appropriately, including interruption or discontinuation of BLINCYTO® as
needed.
- Tumor Lysis Syndrome (TLS), which may be life-threatening or fatal, has been
observed. Preventive measures, including pretreatment nontoxic cytoreduction and
on-treatment hydration, should be used during BLINCYTO®
treatment. Monitor patients for signs and symptoms of TLS and interrupt or
discontinue BLINCYTO® as needed to manage these events.
- Neutropenia and Febrile Neutropenia, including life-threatening cases, have been
observed. Monitor appropriate laboratory parameters (including, but not limited
to, white blood cell count and absolute neutrophil count) during BLINCYTO®
infusion and interrupt BLINCYTO® if prolonged neutropenia occurs.
- Effects on Ability to Drive and Use Machines: Due to the possibility of
neurological events, including seizures and ICANS, patients receiving
BLINCYTO® are at risk for loss of consciousness, and
should be advised against driving and engaging in hazardous occupations or
activities such as operating heavy or potentially dangerous machinery while
BLINCYTO® is being administered.
- Elevated Liver Enzymes: Transient elevations in liver enzymes have been
associated with BLINCYTO® treatment with a median time
to onset of 3 days. In patients receiving BLINCYTO®,
although the majority of these events were observed in the setting of CRS, some
cases of elevated liver enzymes were observed outside the setting of CRS, with a
median time to onset of 19 days. Grade 3 or greater elevations in liver enzymes
occurred in approximately 7% of patients outside the setting of CRS and resulted
in treatment discontinuation in less than 1% of patients. Monitor ALT, AST,
gamma-glutamyl transferase, and total blood bilirubin prior to the start of and during
BLINCYTO® treatment. BLINCYTO®
treatment should be interrupted if transaminases rise to > 5 times the upper
limit of normal (ULN) or if total bilirubin rises to > 3 times ULN.
- Pancreatitis: Fatal pancreatitis has been reported in patients receiving
BLINCYTO® in combination with dexamethasone in clinical
trials and the post-marketing setting. Evaluate patients who develop signs and
symptoms of pancreatitis and interrupt or discontinue BLINCYTO® and
dexamethasone as needed.
- Leukoencephalopathy: Although the clinical significance is unknown, cranial
magnetic resonance imaging (MRI) changes showing leukoencephalopathy have been
observed in patients receiving BLINCYTO®, especially in
patients previously treated with cranial irradiation and antileukemic
chemotherapy.
- Preparation and administration errors have occurred with BLINCYTO® treatment.
Follow instructions for preparation
(including admixing) and administration in the PI strictly to minimize
medication errors (including underdose and overdose).
- Immunization: Vaccination with live virus vaccines is not recommended for at
least 2 weeks prior to the start of BLINCYTO®
treatment, during treatment, and until immune recovery following last cycle of
BLINCYTO®.
- Benzyl Alcohol Toxicity in Neonates: Serious adverse reactions, including fatal
reactions and the “gasping syndrome,” have been reported in very low birth
weight (VLBW) neonates born weighing less than 1500 g, and early preterm
neonates (infants born less than 34 weeks gestational age) who received
intravenous drugs containing benzyl alcohol as a preservative. Early preterm
VLBW neonates may be more likely to develop these reactions, because they may be
less able to metabolize benzyl alcohol.
Use the preservative-free
preparations of BLINCYTO® where possible in
neonates. When prescribing BLINCYTO® (with
preservative) for neonatal patients, consider the combined daily metabolic
load of benzyl alcohol from all sources including BLINCYTO® (with
preservative), other products containing
benzyl alcohol or other excipients (e.g., ethanol, propylene glycol) which
compete with benzyl alcohol for the same metabolic pathway.
Monitor neonatal patients
receiving BLINCYTO® (with preservative) for new or
worsening metabolic acidosis. The minimum amount of benzyl alcohol at which
serious adverse reactions may occur in neonates is not known. The
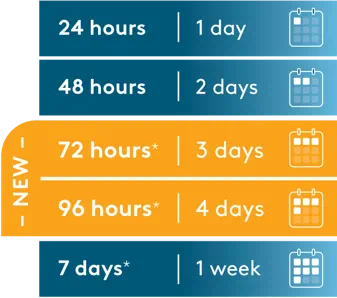
BLINCYTO® 72-Hour bag (with preservative) and 96-Hour bag (with preservative) contain 2.5 mg of benzyl alcohol per mL, and the 7-Day bag (with preservative) contains
7.4 mg of benzyl alcohol per mL.
- Embryo-Fetal Toxicity: Based on its mechanism of action, BLINCYTO® may cause
fetal harm when administered to a pregnant
woman. Advise
pregnant women of the potential risk to the fetus. Advise females of
reproductive potential to use effective contraception during treatment with
BLINCYTO® and for 48 hours after the last dose.
Adverse Reactions
-
The safety of BLINCYTO® in adult and pediatric patients one month and older with MRD-positive B-cell precursor
ALL (n=137), relapsed or refractory B-cell precursor ALL (n=267), and Philadelphia chromosome-negative B-cell
precursor ALL in consolidation (n=165) was evaluated in clinical studies. The most common adverse reactions (≥
20%) to BLINCYTO® in this pooled population were pyrexia, infusion-related reactions, headache, infection, musculoskeletal pain, neutropenia, nausea, anemia, thrombocytopenia, and diarrhea.
Dosage and Administration Guidelines
- BLINCYTO® is administered as a continuous intravenous
infusion at a constant flow rate using an infusion pump which should be
programmable, lockable, non-elastomeric, and have an alarm.
- It is very important that the instructions for preparation (including admixing)
and administration provided in the full Prescribing Information are strictly
followed to minimize medication errors (including underdose and overdose).
INDICATIONS
BLINCYTO® (blinatumomab) is indicated for the treatment of CD19-positive B-cell precursor acute lymphoblastic leukemia (ALL) in adult and pediatric patients one month and older with:
- Philadelphia chromosome-negative disease in the consolidation phase of multiphase chemotherapy
-
Minimal residual disease (MRD) greater than or equal to 0.1% in first or second complete remission
-
Relapsed or refractory disease
Please see BLINCYTO® full Prescribing Information,
including BOXED WARNINGS.
BLINCYTO® is a registered trademark of Amgen
Inc.