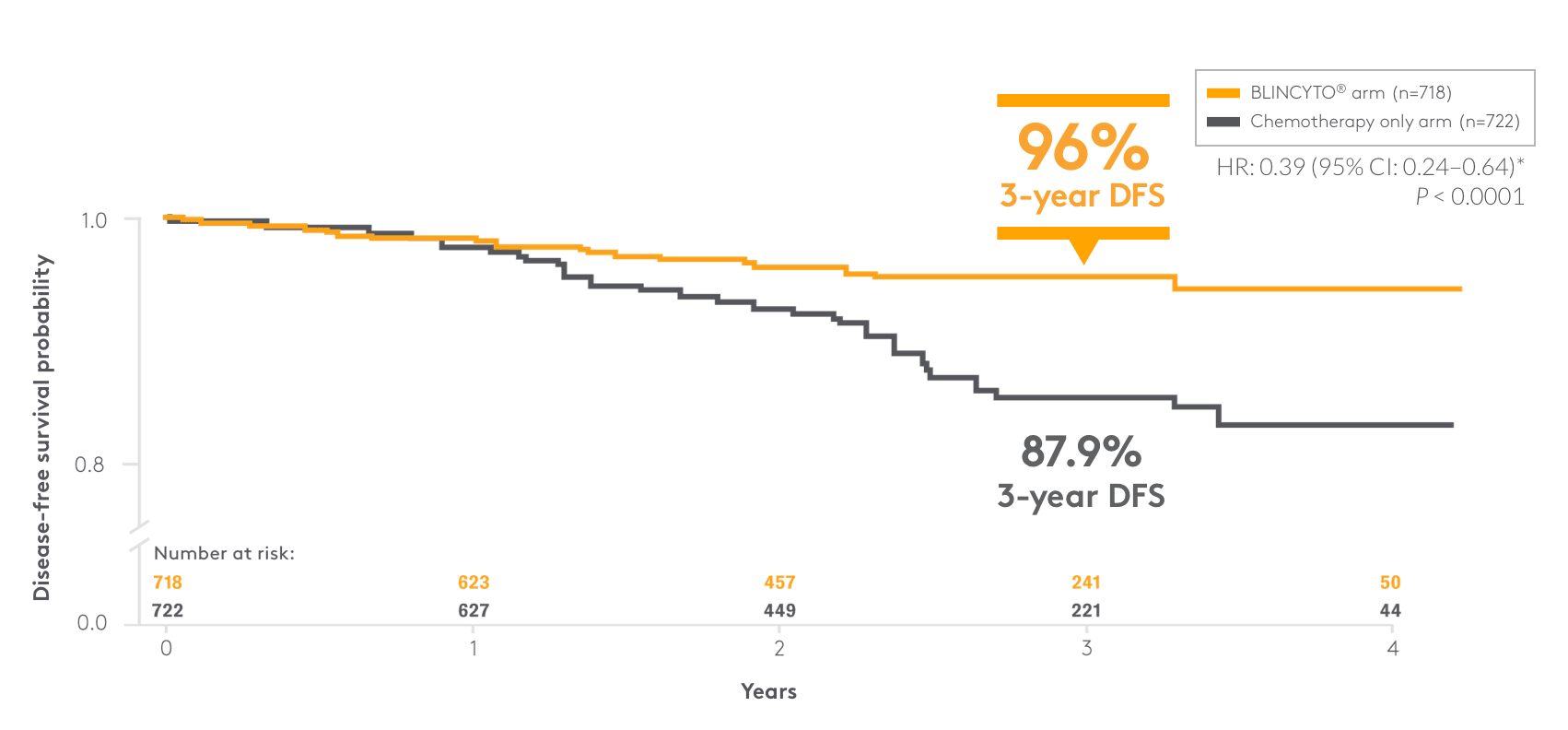
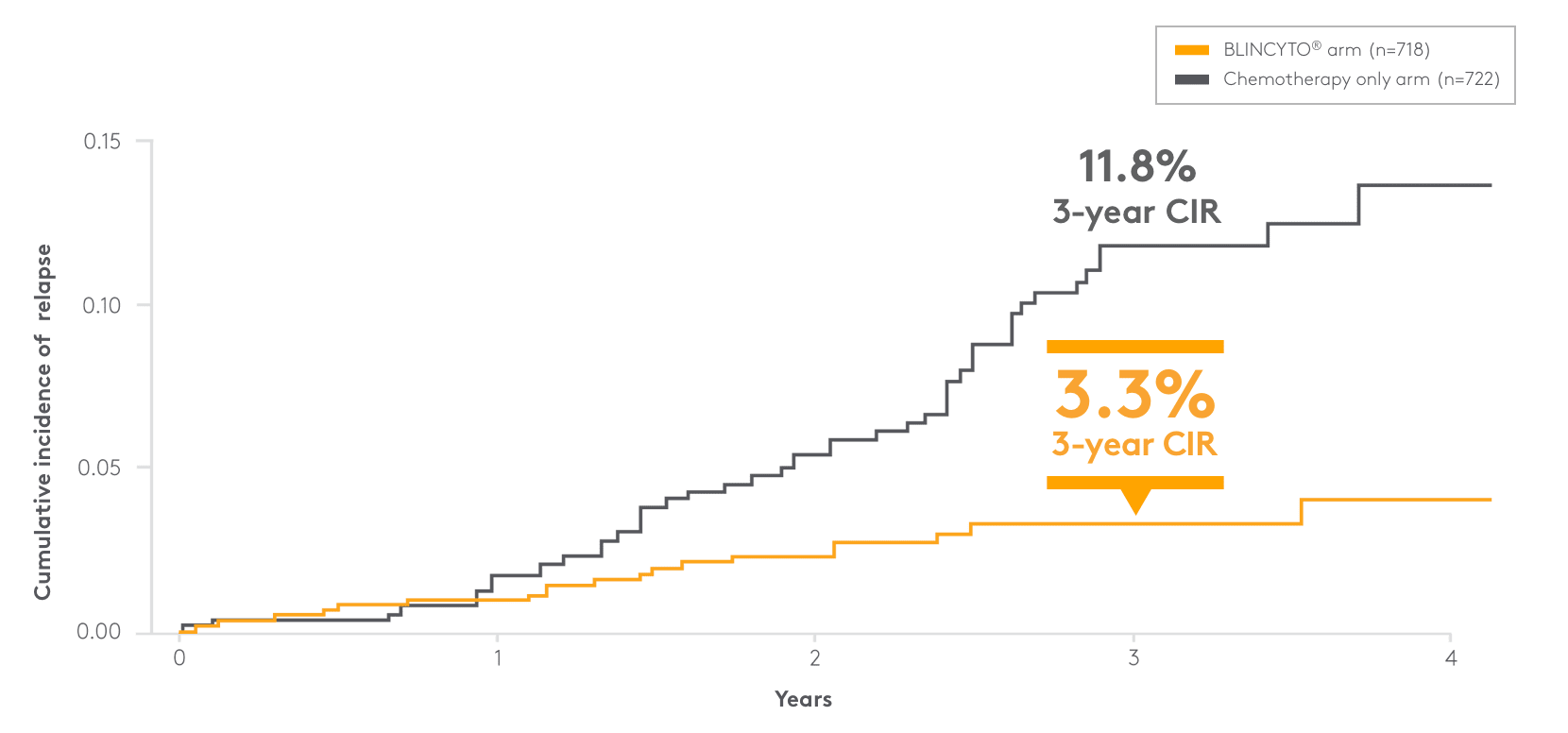
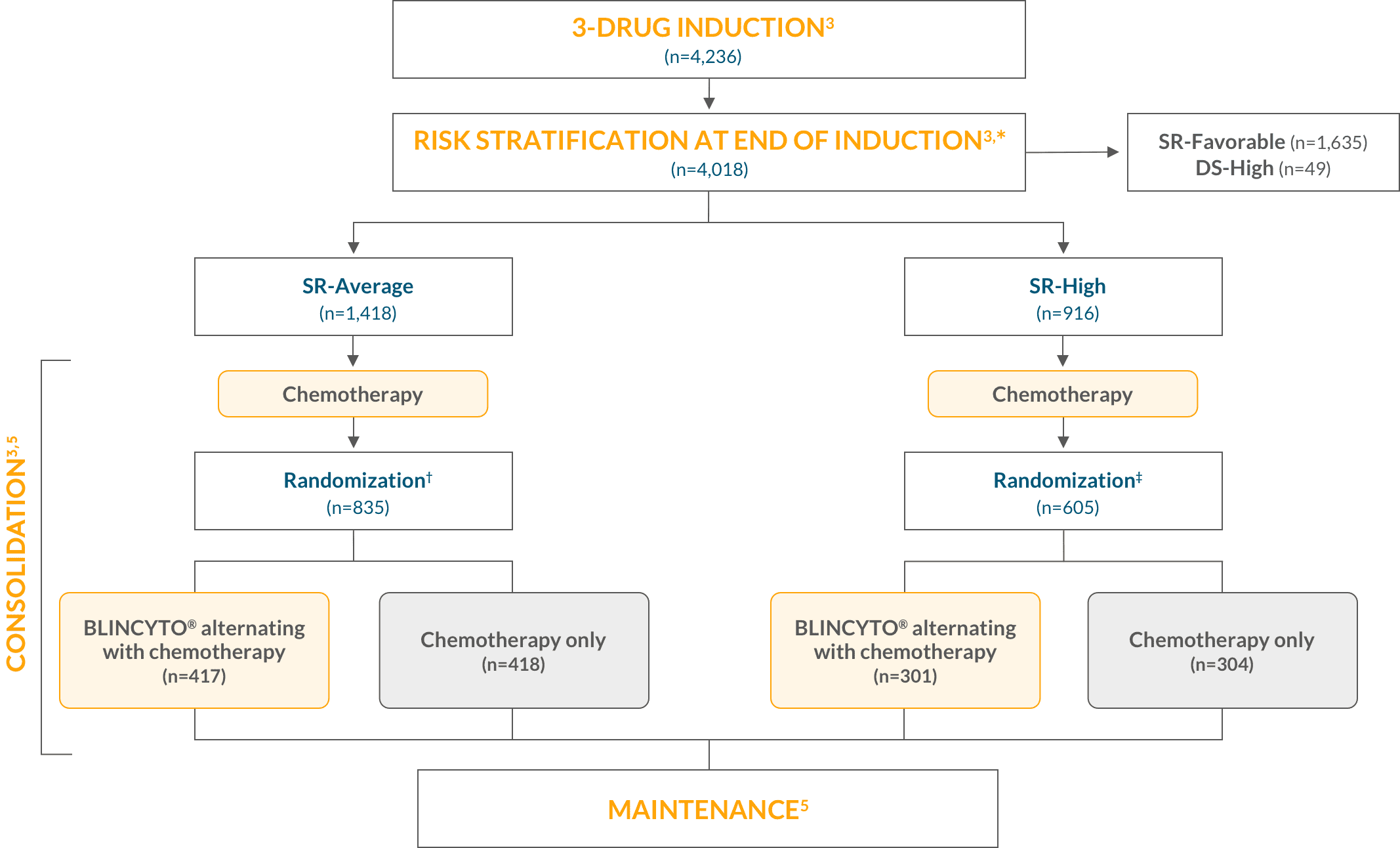
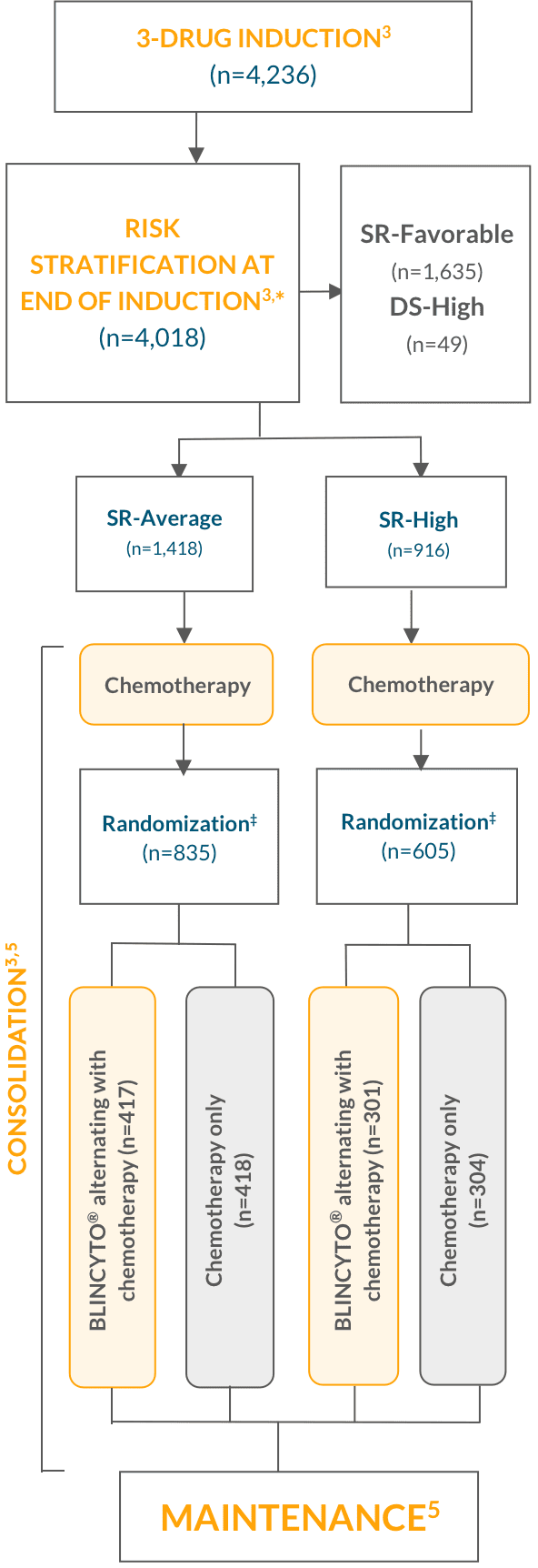
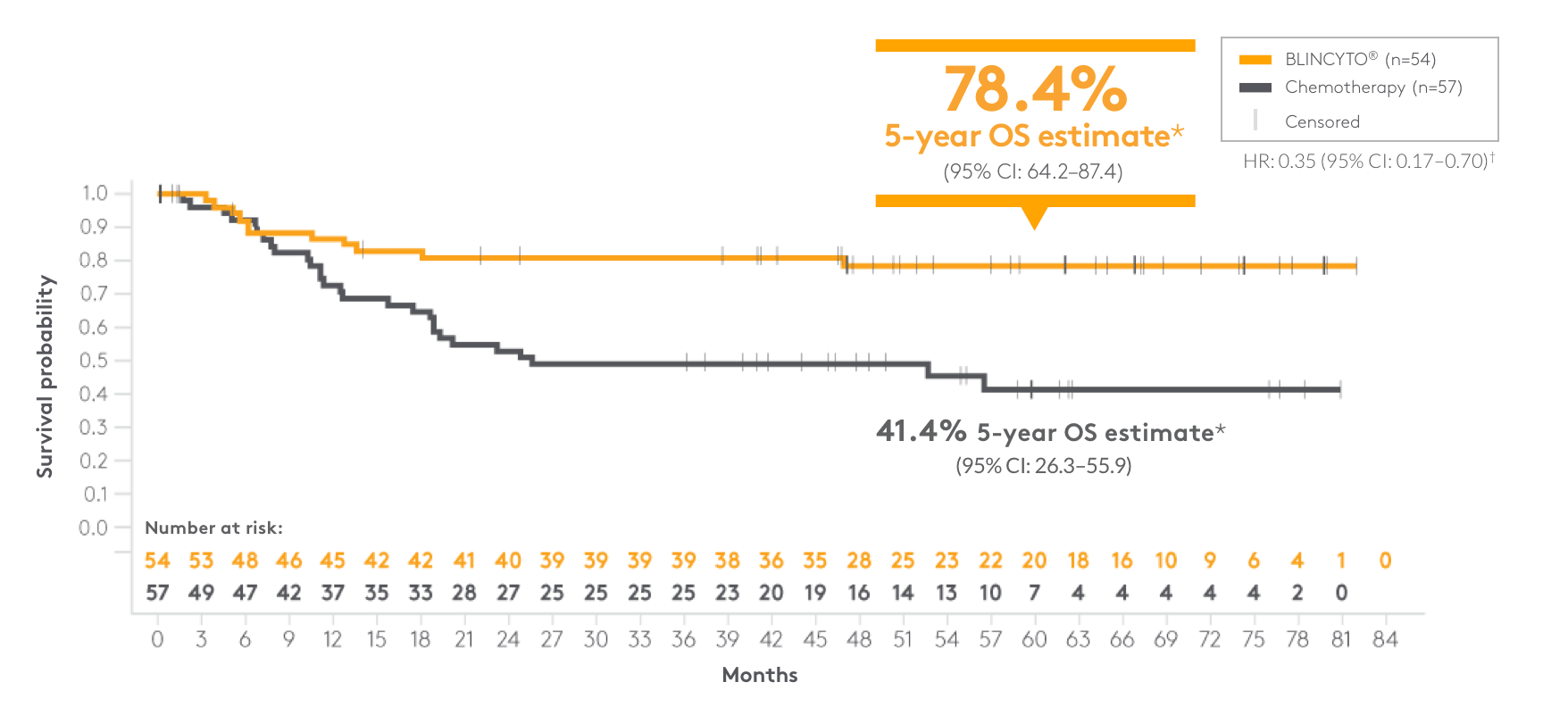
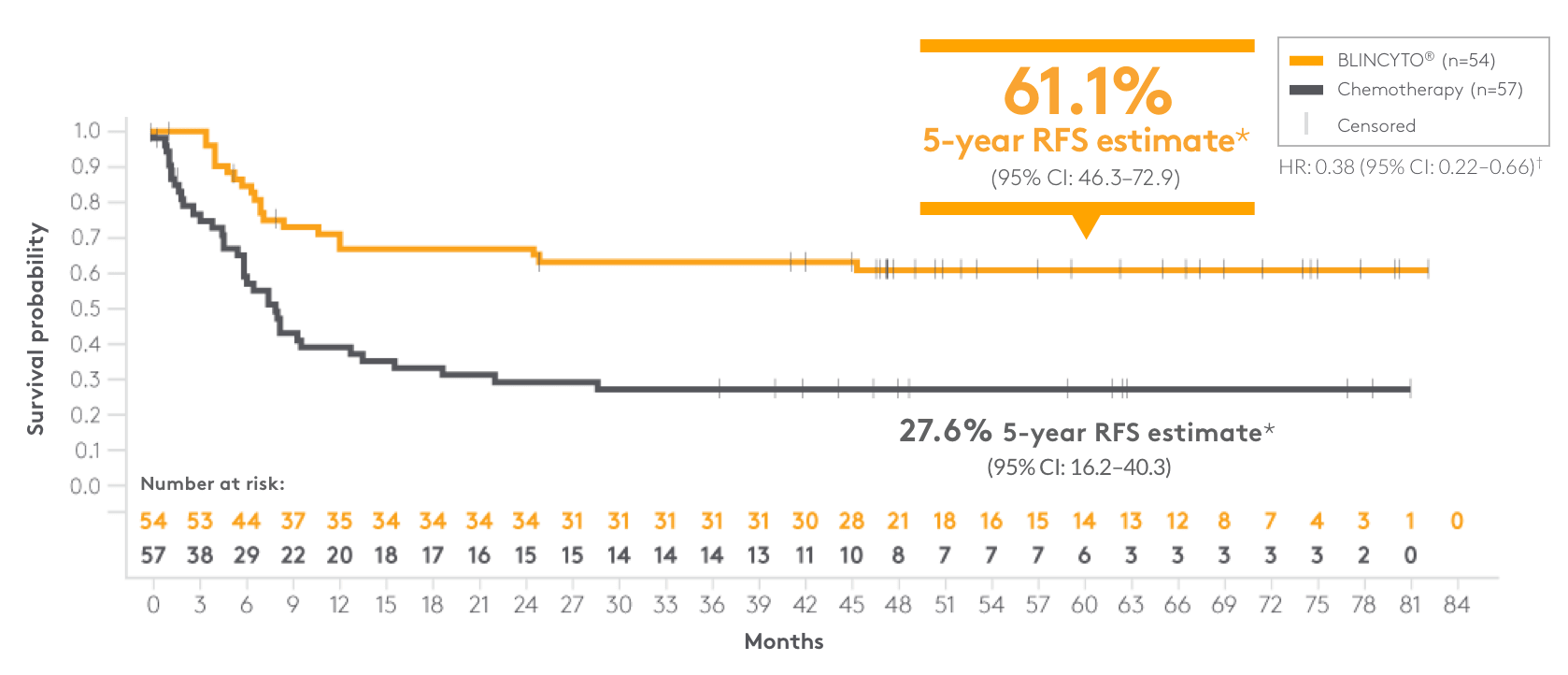
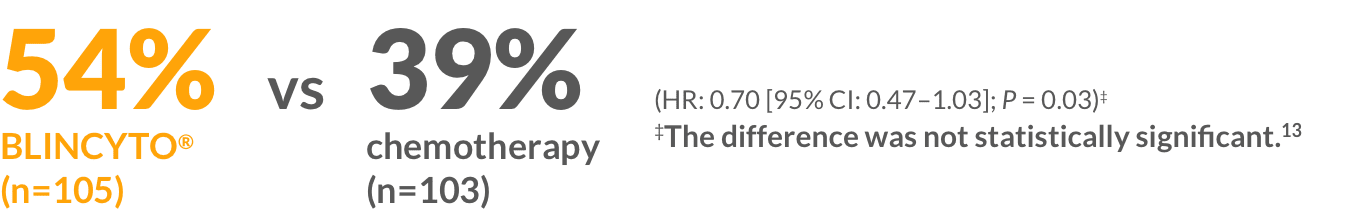
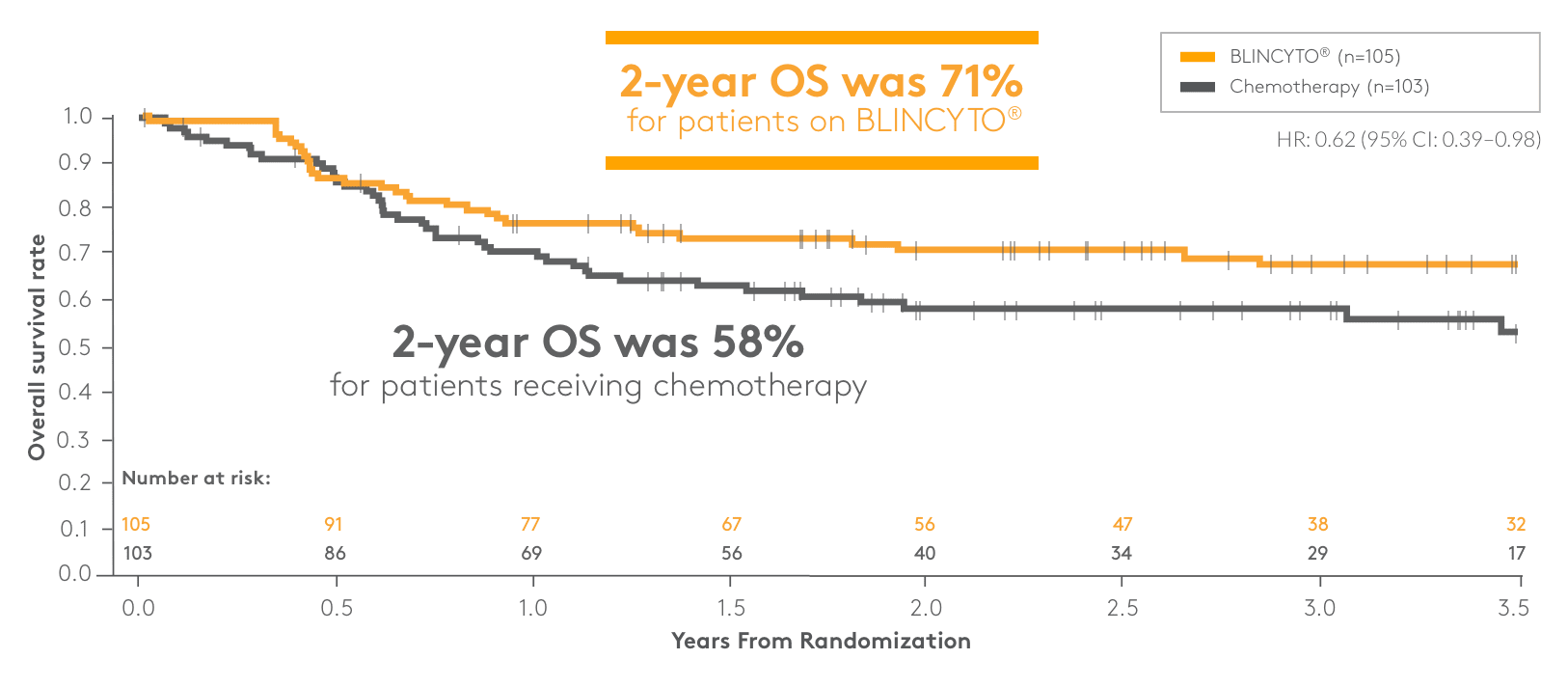
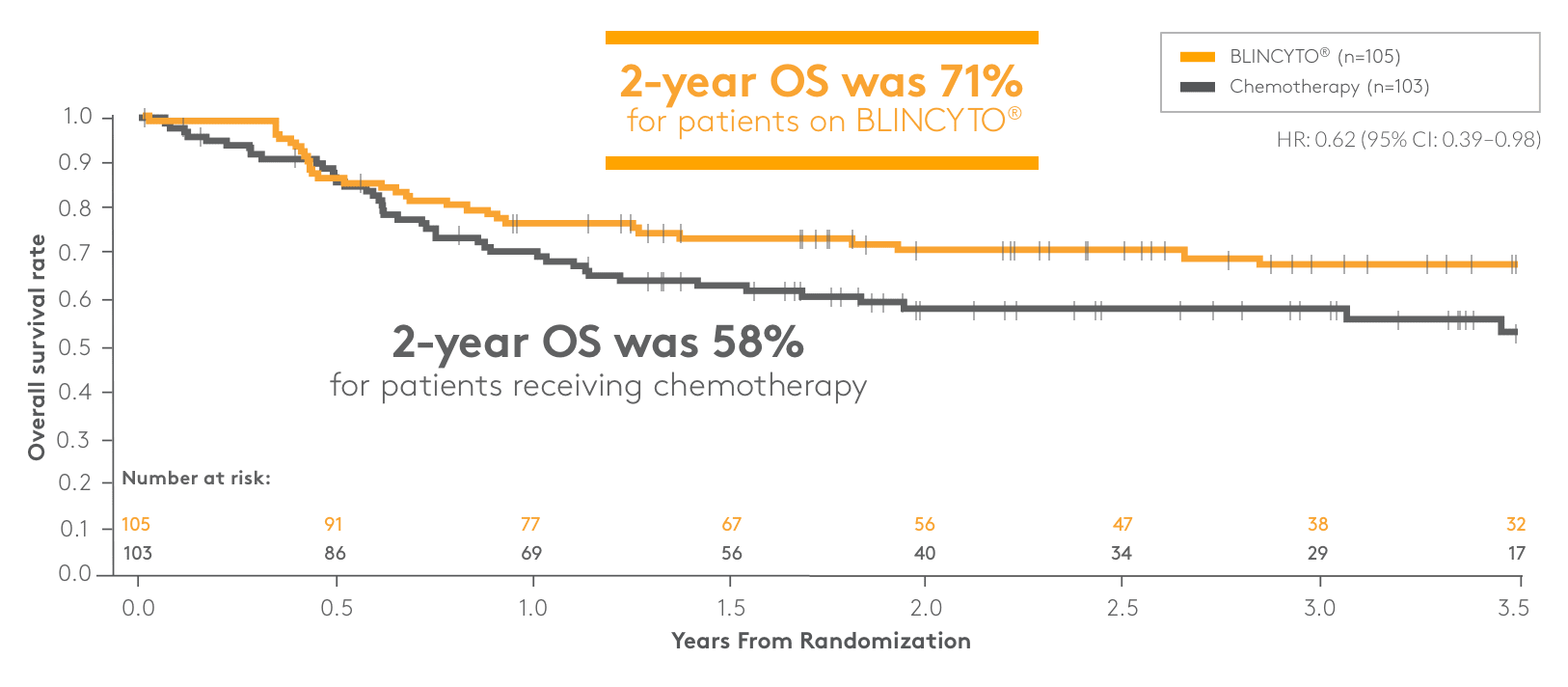
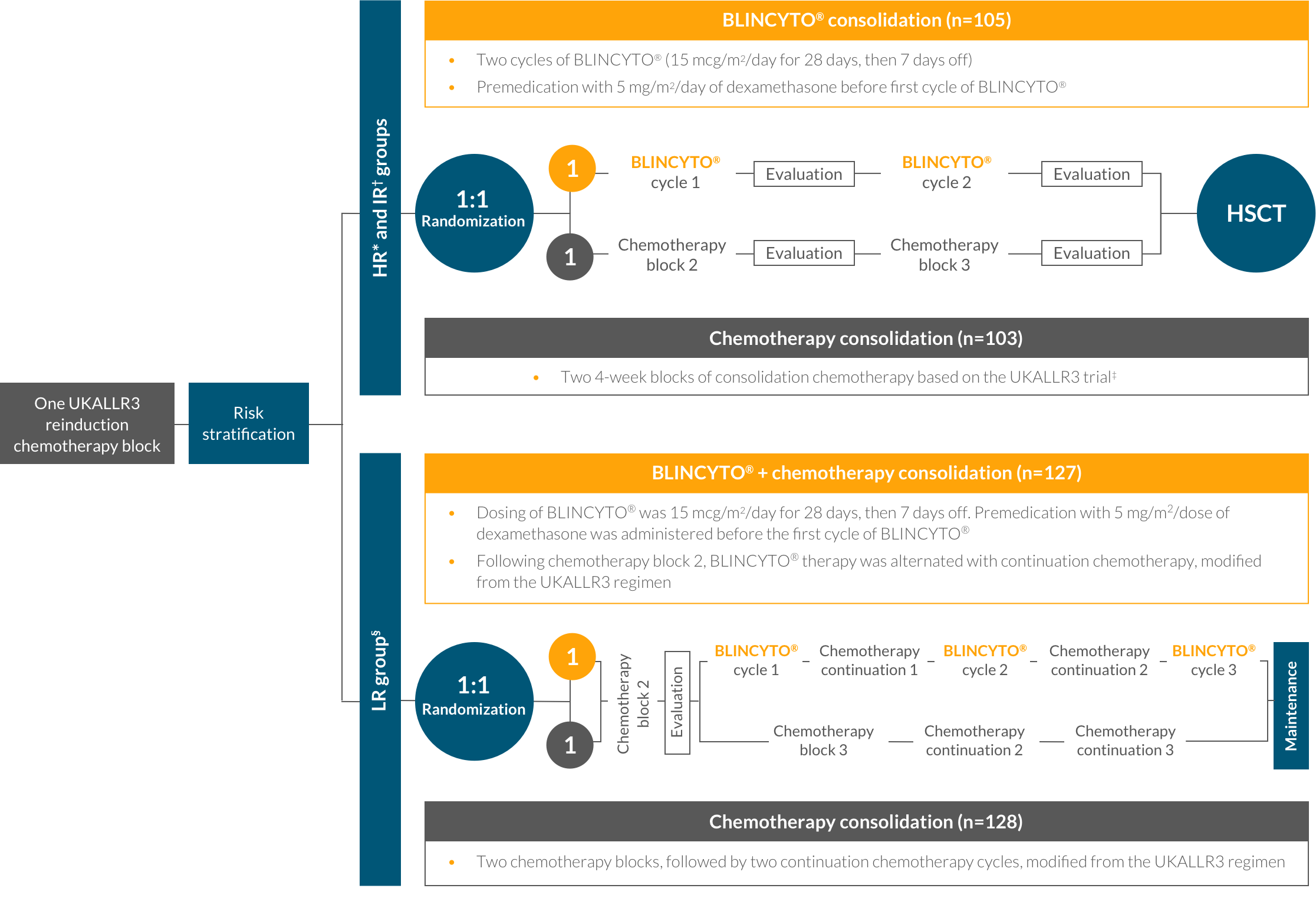
References: 1. BLINCYTO® (blinatumomab) prescribing information, Amgen. 2. Litzow MR, Sun Z, Mattison RJ, et al. Blinatumomab for MRD-negative acute lymphoblastic leukemia in adults. N Engl J Med. 2024;391:320-333. 3. Gupta S, Rau RE, Kairalla JA, et al. Blinatumomab in standard-risk B-cell acute lymphoblastic leukemia in children. N Engl J Med. Published online December 7, 2024. doi:10.1056/NEJMoa2411680. 4. Rau R, Gupta S, Kairalla J, Rabin K, Loh M, Raetz E. Blinatumomab added to chemotherapy improves disease-free survival in newly diagnosed NCI standard risk pediatric B-acute lymphoblastic leukemia: Results from Children’s Oncology Group Study AALL1731. Presented at: 66th ASH Annual Meeting and Exposition; December 7–10, 2024; San Diego, CA. 5. Gupta S, Rau RE, Kairalla JA, et al. Blinatumomab in standard-risk B-cell acute lymphoblastic leukemia in children. N Engl J Med. Published online December 7, 2024 (suppl). doi:10.1056/NEJMoa2411680. 6. Brazauskas R, Eapen M, Wang T. Endpoint selection and evaluation in hematology studies. Best Pract Res Clin Haematol. 2023;36:101479. 7. Gupta S, Rau RE, Kairalla JA, et al. Blinatumomab in standard-risk B-cell acute lymphoblastic leukemia in children. N Engl J Med. Published online December 7, 2024 (protocol). doi:10.1056/NEJMoa2411680. 8. Data on file, Amgen; 2020. 9. Locatelli F, Zugmaier G, Rizzari C, et al. Effect of blinatumomab vs chemotherapy on event-free survival among children with high-risk first-relapse B-cell acute lymphoblastic leukemia: a randomized clinical trial. JAMA. 2021;325:843-854. 10. Locatelli F, Zugmaier G, Rizzari C, et al. Effect of blinatumomab vs chemotherapy on event-free survival among children with high-risk first-relapse B-cell acute lymphoblastic leukemia: a randomized clinical trial. JAMA. 2021;325(suppl 3):843-854. 11. Locatelli F, Zugmaier G, Rizzari C, et al. Effect of blinatumomab vs chemotherapy on event-free survival among children with high-risk first-relapse B-cell acute lymphoblastic leukemia: a randomized clinical trial. JAMA. 2021;325(suppl):843-854. 12. Brown PA, Ji L, Xu X, et al. Effect of postreinduction therapy consolidation with blinatumomab vs chemotherapy on disease-free survival in children, adolescents, and young adults with first relapse of B-cell acute lymphoblastic leukemia: a randomized clinical trial. JAMA. 2021;325(suppl 2):833-842. 13. Brown PA, Ji L, Xu X, et al. Effect of postreinduction therapy consolidation with blinatumomab vs chemotherapy on disease-free survival in children, adolescents, and young adults with first relapse of B-cell acute lymphoblastic leukemia: a randomized clinical trial. JAMA. 2021;325:833-842. 14. Hogan LE, Brown PA, Ji L, et al. Children’s Oncology Group AALL1331: Phase III trial of blinatumomab in children, adolescents, and young adults with low-risk B-cell ALL in first relapse. J Clin Oncol. 2023. doi:10.1200/JCO.22.02200. 15. Parker C, Waters R, Leighton C, et al. Effect of mitoxantrone on outcome of children with first relapse of acute lymphoblastic leukaemia (ALL R3): an open-label randomized trial. Lancet. 2010;376:2009-2017. 16. Brown PA, Ji L, Xu X, et al. Effect of postreinduction therapy consolidation with blinatumomab vs chemotherapy on disease-free survival in children, adolescents, and young adults with first relapse of B-cell acute lymphoblastic leukemia: a randomized clinical trial. JAMA. 2021;325(suppl):833-842. 17. von Stackelberg A, Locatelli F, Zugmaier G, et al. Phase I/phase II study of blinatumomab in pediatric patients with relapsed/refractory acute lymphoblastic leukemia. J Clin Oncol. 2016;34:4381-4389. 18. Gökbuget N, Dombret H, Bonifacio M, et al. Blinatumomab for minimal residual disease in adults with B-cell precursor acute lymphoblastic leukemia. Blood. 2018;131:1522-1531. 19. Keating AK, Gossai N, Phillips CL, et al. Reducing minimal residual disease with blinatumomab prior to HCT for pediatric patients with acute lymphoblastic leukemia. Blood Adv. 2019;3:1926-1929. 20. ClinicalTrials.gov.
https://classic.clinicaltrials.gov/ct2/results?term=blinatumomab&cond=Residual+Disease%2C+Minimal&recrs=b&recrs=a&recrs=f&recrs=d&age_v=&gndr=&type=Intr&rslt=&Search=Apply. Accessed January 3, 2025. 21. Referenced with permission from the NCCN Clinical Practice Guidelines in Oncology (NCCN Guidelines®) for Pediatric Acute Lymphoblastic Leukemia V.2.2025. © National Comprehensive Cancer Network, Inc. 2024. All rights reserved. Accessed January 3, 2025. To view the most recent and complete version of the guideline, go online to NCCN.org. NCCN makes no warranties of any kind whatsoever regarding their content, use or application and disclaims any responsibility for their application or use in any way.